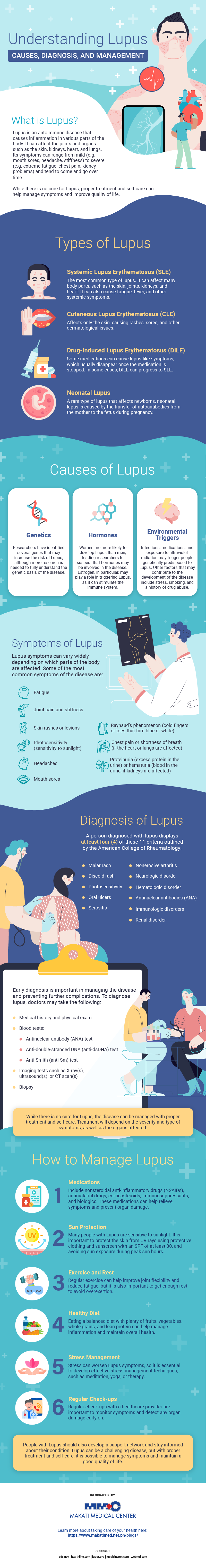
Lupus is a chronic autoimmune disease that affects millions of people worldwide, including Filipinos. Despite its prevalence, lupus remains a misunderstood and often misdiagnosed condition, leading to delays in treatment and increased morbidity and mortality.
The most common symptoms experienced by those with lupus include joint pain and stiffness, rashes, fatigue, and fever. Additionally, lupus can affect various organs in the body, such as the kidneys and heart, leading to potentially life-threatening complications if left untreated.
To improve understanding of lupus and similarly increase awareness about it, here’s an informative guide on its causes, diagnosis, and management.
What is Lupus?
Lupus is a chronic autoimmune disease that can affect many body parts, including the skin, joints, kidneys, and heart. With this disease, people’s immune systems mistakenly attack healthy tissues and organs causing inflammation and damage.
Lupus is a complex disease that can be difficult to diagnose, as its symptoms can mimic those of other conditions.
Types of Lupus
Lupus can present itself in different ways. Below are its four main types:
1. Systemic Lupus Erythematosus (SLE)
The most common type of lupus, SLE can affect many body parts such as the skin, joints, kidneys, and heart. It can also cause fatigue, fever, and other systemic symptoms.
2. Cutaneous Lupus Erythematosus (CLE)
A type of lupus that affects only the skin, causing rashes, sores, and other dermatological symptoms.
3. Drug-Induced Lupus Erythematosus (DILE)
Some medications can cause lupus-like symptoms, which usually go away once the medication is stopped. However, in some cases, DILE can progress to SLE.
4. Neonatal Lupus
A rare type of lupus that affects newborns, neonatal lupus is caused by the transfer of autoantibodies from the mother to the fetus during pregnancy.
Causes of Lupus
While the exact cause of lupus is unknown, researchers believe that a combination of genetic and environmental factors can trigger the disease. Here are some of the factors that may contribute to its development:
- Genetics
Lupus can run in families, suggesting that genetic factors play a role in the disease. Researchers have identified several genes that may increase the risk of lupus, although more research is needed to fully understand the genetic basis of the disease.
- Hormones
Women are more likely to develop lupus than men, leading researchers to suspect that hormones may be involved in the disease. Estrogen, in particular, may play a role in triggering lupus, as it can stimulate the immune system.
- Environmental triggers
Certain environmental triggers, such as infections, medications, and exposure to ultraviolet radiation, may trigger people genetically predisposed to the disease. For example, a viral infection may activate the immune system and trigger the production of autoantibodies that attack healthy tissues. Other factors that may contribute to the development of lupus include stress, smoking, and a history of drug abuse.
Understanding the factors that possibly trigger lupus can help people diagnosed with it manage their symptoms and reduce the risk of complications.
Symptoms of Lupus
Although symptoms of lupus can vary widely from person to person, here are some of the most common ones:
- Fatigue: Extreme tiredness or fatigue among people with lupus can result from the disease itself or a side effect of medication.
- Joint pain and stiffness: Joint pain and stiffness can affect any part of the body, including the fingers, wrists, knees, and ankles.
- Skin rashes or lesions: One of the first signs of lupus is the development of a butterfly-shaped rash across the cheeks and nose. Other types of rashes and lesions can also occur.
- Photosensitivity: Many people with lupus are sensitive to sunlight, which can trigger or worsen symptoms.
- Headaches: Headaches are common in people with lupus and can result from inflammation or medications.
- Mouth sores: Mouth sores, also known as oral ulcers, can be a common symptom of lupus.
- Raynaud’s phenomenon: Raynaud’s phenomenon is a condition wherein the fingers or toes turn blue or white in response to cold or stress.
- Chest pain or shortness of breath: If lupus affects the heart or lungs, chest pain or shortness of breath can occur.
- Proteinuria or hematuria: If lupus affects the kidneys, excess protein or blood may be present in the urine.
Note that not everyone with lupus will experience all of these symptoms, and their severity can also vary over time. Should you experience any of these symptoms, talk to your healthcare provider to determine the cause and develop an appropriate treatment plan.
Diagnosis of Lupus
When a person has at least four of these 11 criteria established by the American College of Rheumatology, they can be officially diagnosed with lupus:
- Malar rash
- Discoid rash
- Photosensitivity
- Oral ulcers
- Nonerosive arthritis
- Serositis
- Renal disorder
- Neurologic disorder
- Hematologic disorder
- Antinuclear antibodies (ANA)
- Immunologic disorders
Diagnosing lupus can be challenging, as many symptoms can mimic those of other conditions. However, early diagnosis is important for managing the disease and preventing complications. Here are some of the steps that doctors may take to diagnose lupus:
- Medical history and physical exam: Doctors will begin by taking a detailed medical history and conducting a physical exam to check for signs and symptoms of lupus.
- Blood tests: Blood tests can help doctors look for specific antibodies and other markers of autoimmune disease. Some of the blood tests that may be done to diagnose lupus include:
- Antinuclear antibody (ANA) test: This test looks for antibodies that attack the nucleus of cells, a common feature of lupus.
- Anti-double-stranded DNA (anti-dsDNA) test: This test looks for antibodies that attack double-stranded DNA, which is also commonly found in people with lupus.
- Anti-Smith (anti-Sm) test: This test looks for antibodies that attack a specific protein found in the nucleus of cells, which is highly specific to lupus.
- Imaging tests: Imaging tests, such as X-rays, ultrasounds, or CT scans, may be used to check for damage to internal organs, such as the kidneys or lungs.
- Biopsy: In some cases, doctors may perform a biopsy, wherein a small tissue sample is examined under a microscope. This can help doctors confirm a lupus diagnosis and determine the extent of organ damage.
Treatment and Management of Lupus
While there is no cure for lupus, the disease can be managed with proper treatment and self-care. Treatment for lupus will depend on the severity and type of symptoms, as well as the organs affected. Here are some of the most common ways to manage lupus:
1. Medications
Medications that can be used to treat lupus include nonsteroidal anti-inflammatory drugs (NSAIDs), antimalarial drugs, corticosteroids, immunosuppressants, and biologics, which can help relieve symptoms and prevent organ damage.
2. Sun protection
Many people with lupus are sensitive to sunlight, so it is important to protect the skin from UV rays. This can include wearing protective clothing, using sunscreen with an SPF of at least 30, and avoiding sun exposure during peak hours.
3. Exercise and rest
Regular exercise can help improve joint flexibility and reduce fatigue, but it is also important to get enough rest and avoid overexertion.
4. Healthy diet
Eating a balanced diet with plenty of fruits, vegetables, whole grains, and lean protein can help manage inflammation and maintain overall health.
5. Stress management
Stress can worsen lupus symptoms, so it is essential to develop effective stress management techniques, such as meditation, yoga, or therapy.
6. Regular check-ups
Regular check-ups with a healthcare provider are important to monitor symptoms and detect any organ damage early on.
In addition to these treatments, people with lupus need to develop a support network and stay informed about their condition. Lupus can be a challenging disease, but with proper treatment and self-care, it is possible to manage symptoms and maintain a good quality of life.
Beyond the Diagnosis: Navigating Life with Lupus
Lupus can affect many parts of the body, and its symptoms can vary widely from person to person—making diagnosis challenging. While the exact cause of lupus is still unknown, research has revealed that a combination of genetic, hormonal, and environmental factors may play a role.
Living with lupus can be challenging. However, with proper treatment and self-care, it is possible to manage symptoms and maintain a good quality of life. If you or someone you know is experiencing symptoms of lupus, it is important to talk to a healthcare provider and get the necessary support and resources. By staying informed and developing a support network, people with lupus can lead fulfilling and healthy lives.
Find expert rheumatology care and support at Makati Medical Center. Schedule an appointment with us and learn more about managing lupus and other autoimmune diseases.