Patient Reference
- Home
- Patient And Visitor Guide
- Patient Reference

YOUR RIGHTS AS A PATIENT
As a patient at Makati Medical Center, we strive to keep you well informed, encourage participation in your treatment choices, and promote continuous open communication with your health care team. As a patient and partner, we encourage you to learn about patient rights and responsibilities during your stay at our hospital.
(World Medical Association Declaration of Rights of the Patient – Adopted from the 34th World Medical Assembly Lisbon, Portugal, September/October 1981 and amended by the 47th General Assembly Bali, Indonesia, September 1995 and Magna Carta of Patient’s Rights and Obligations of 2008- Senate Bill 2371)
- Right to Good Quality Health Care and Humane Treatment
Every person has a right to a continuity of good quality Health Care without discrimination and within the limits of the resources, manpower and competence available for health and medical care. In the course of such care, his human dignity, convictions, integrity, individual needs and culture shall be respected.
- Right to Dignity
The Patient’s dignity, culture and value shall be respected at all times in medical care and teaching. Likewise, terminally ill patients shall be entitled to humane terminal care to make dying as dignified and comfortable as possible.
- Right to choose his Physician/ Health Institution
The Patient is free to choose the services of a physician or health institution of his choice except when he chooses to be confined in a charity ward. In this case, the attending physician shall be the consultant under whose service the patient was admitted as appearing in the Doctor’s Order Sheet of the Medical Record. The Patient shall have the right to seek a second opinion and subsequent opinions, if necessary, from another physician or health institution, and to change his physician or health institution.
- Right to Informed Consent
The Patient has a right to self- determination and to make free decisions regarding himself / herself. However, the attending physician shall inform the Patient of the consequences of his/her decisions.- Rights of Unconscious Patients
If the patient is unconscious or otherwise unable to express his/her will, informed consent must be obtained whenever possible, from a legally entitled representative.If a legally entitled representative is not available, and a medical intervention is urgently needed, consent of the patient may be presumed, unless it is obvious and beyond doubt on the basis of the patient’s previous firm expression or conviction that he/she would refuse consent. In all cases, a physician always strives to save the life of a patient unless a prior explicit written document states otherwise (Do Not Resuscitate). - Rights of Legally Incompetent Patient
If a patient is a minor or otherwise legally incompetent, the consent of a legally entitled representative is required. Nevertheless, the patient must be involved in the decision making to the fullest extent allowed by his/her capacity or circumstance.If a legally incompetent patient can make rational choices, decisions must be respected and he/she has the right to forbid disclosure of information to his/her legally entitled representative.
If the patient’s legally entitled representative, (a person authorized by the patient), forbids treatment which is, in the opinion of the physician, in the patient’s best interest, the physician should challenge this decision before the proper forum. In case of emergency, the physician will act in the patient’s best interest. Procedures against the Patient’s Will
Diagnostic procedures or treatments against the patient’ s will can be carried out only in exceptional cases, if specifically permitted by law and conforming to the principles of medical ethics. In such cases, informed consent is secured from next-of-kin whenever possible.
- Rights of Unconscious Patients
- Right to Refuse Diagnostic and Medical Treatment
The Patient has the right to refuse diagnostic and medical treatment procedures, provided that the following conditions are satisfied;
- The Patient is of legal age and is mentally competent;
- The Patient is informed of the medical consequences of his/her refusal;
- The Patient releases those involved in his care from any obligation relative to the consequences of his/her decision; and
- The Patient’s refusal will not jeopardize public health and safety.
- Right to Refuse Participation in Medical Research
The Patient has the right to be advised of plans to involve him/her in medical research that may affect the care or treatment of his/her condition. Any proposed research shall be performed only upon the written informed consent of the Patient. - Right to Religious Belief and Assistance
The Patient has the right to receive spiritual and moral comfort, including the help of a priest or minister of his/her chosen religion. He/ she also has the right to refuse medical treatment or procedures which may be contrary to his religious beliefs, subject to the limitations described in number 5. - Right to Privacy and Confidentiality
The patient has the right to privacy and protection from unwarranted publicity. The right to privacy shall include the patient’s right not to be subjected to exposure, private or public, either by photography, publications, video-taping, discussion, or by any other means that would otherwise tend to reveal his person and identity and the circumstances under which he was, he is, or he will be, under medical or surgical care or treatment. - Right to Disclosure Of, And Access To, Information
In the course of the patient’s treatment and hospital care, the Patient or his/her legal guardian has the right to be informed of the result of the evaluation of the nature and extent of his/her disease. Any other additional or further contemplated medical treatment on surgical procedure or procedures, shall be disclosed and may only be performed with the written consent of the patient. - Right to Health Education
Every patient has the right to health education that will assist him/her in making informed choices about personal health and about available health services. The education shall include information about healthy lifestyles and about methods of prevention and early detection of illnesses. The personal responsibility of everybody for his own health should be stressed. - Right to Correspondence and To Receive Visitors
The Patient has the right to communicate with his/her relatives and other persons and to receive visitors. MMC visitation guidelines are implemented considering the benefit of visitation to the patient; impact of visitation on patient care and the safety and security of patients, visitors and all healthcare workers. - Right to Medical Records
Makati Medical Center and the physician shall ensure and safeguard the integrity and authenticity of the medical records. The Patient, upon his/her request, is entitled to a medical certificate and clinical abstract. He/she has the right to view, and obtain an explanation of, the contents of his/her medical records from the attending physician, except for psychiatric notes and other incriminating information obtained about a third party. Any relevant document that the Patient may require for insurance claims shall be made available to him within a reasonable period of time. - Right to Leave Against Medical Advise
The Patient has the right to leave Makati Medical Center regardless of his/her physical condition, Provided, That:
- He/she is informed of the medical consequences of his/her decision;
- He/she releases those involved in his/her care from any obligation relative to the consequences of his/her decision; and
- His/her decision will not prejudice public health and safety
- Right to Express Grievances
Every Patient has the right to express valid complaints and grievances about the care and services received and to know the disposition of such complaints. - Right to be informed of His Rights and Obligations as a PatientEvery Patient has the right to be informed of his/her rights and obligations as a Patient. It shall also be the duty of Makati Medical Center to inform Patients of their rights as well as Makati Medical Center’s rules and regulations that apply to the conduct of the Patient while in the care of such institution.
YOUR OBLIGATIONS AS A PATIENT
As a patient at Makati Medical Center, you and/or your representative are expected to—for optimal and appropriate care:
- Know and exercise your rights as a patient responsibly and reasonably.
- Report to your doctor any unexpected change(s) in your condition or symptoms.
- Ask questions when you do not understand what your doctor or other members of your health care team tell you about diagnosis or treatment and its cost. You should inform your doctor if you anticipate problems in following prescribed treatment and you are considering alternative therapies (may interfere or interact with care).
- Understand and accept the consequences of your informed consent. If you refuse the treatment or advice of the healthcare provider, you must accept the consequences of such decision and relieve the healthcare provider of any liability as a result of the exercise of your right to self-determination.
- Provide complete and accurate information for insurance claims and work with the hospital’s Credit Billing and Collection staff to ensure payment settlement.
- Know your health insurance coverage and related policies concerning required pre-approvals, covered services, admissions, and the hospital and doctors covered by your insurance provider.
- Pay your hospital and physician bills in a timely manner.
- Ask questions from your insurance company or the hospital’s Billing Services if there is a financial issue that you do not understand.
- Maintain a state of wellness and refrain from indulging in unhealthy lifestyle that has adverse impact on your health.
- Provide complete and accurate information about your health, including present condition, past illness(es), hospitalization(s), medication(s), natural products and vitamins, and any other matter that pertains to your health.
- Provide complete and accurate information including your full name, address, home telephone number, date of birth, insurance provider, and employer, when it is necessary.
- Provide your doctor or the hospital with a copy of your Advance Directive if you have one and want it to apply during your admission.
- Ask your doctor or nurse what to expect regarding pain and pain management plan. You should tell your doctor or nurse on any concerns about taking pain medication.
- Respect the physician’s decision to choose whom he/she will treat and his/her religious beliefs. Exercise transparency on all communications between you and your physician.
- Abide by all hospital rules and regulations.
- Comply with the NO SMOKING policy.
- Comply with Visiting Hours and policies to ensure the rights and comfort of all patients. Be considerate of noise levels, privacy and safety. Weapons are prohibited inside hospital premises.
- Treat hospital staff, other patients, and visitors with courtesy and respect.
- Cooperate and participate with your healthcare providers and trainees that may be involved the care process.
- Direct your complaints or questions, to the hospital’s Patient Relations department through [email protected].
- Leave valuables at home and bring only items necessary during your hospital stay.
MakatiMed is one of the pioneers in kidney transplantation in the Philippines, performing this surgery as early as 1970’s. The MakatiMed Transplant Team, medical facilities, and services are readily available and accessible.
WHAT IS KIDNEY TRANSPLANTATION?
A Kidney Transplantion is a surgical procedure that involves the transplantation of a kidney from a living (related or non-related) or deceased (cadaver) donor, to replace the function of the affected kidneys. It is the best option of treatment for patients with end-stage kidney failure. The surgery involves two patients: the recipient and the donor. Before a kidney transplant, both the recipient and the donor are required to undergo extensive medical and psychosocial evaluations. This is to ensure the success of the procedure and safety of both patients.
WHO IS PART OF THE TRANSPLANT TEAM?
A Transplant Team is a group of highly skilled doctors, specialized nurses, and allied healthcare providers who are committed to deliver the highest level of care to the patients involved in a kidney transplant. The team is composed of a Nephrologist, Urologist, Vascular Surgeon, Anesthesiologist, Transplant Coordinator, Transplant Nurse, Psychiatrist, Dietitian, Physiotherapist and Social Workers.
WHAT IS A HOSPITAL TRANSPLANT ETHICS COMMITTEE (HTEC)?
The Hospital Transplant Ethics Committee of Makati Medical Center is an independent body, composed of a group of individuals representing the different sectors of society. It is composed of a Nephrologist, Psychiatrist, Medical Intensivist, Priest, Social Worker, Lawyer, and a Lay Person. The Committee’s primary goal is to ensure the welfare, safety, and rights of patients and the hospital’s adherence to ethical, moral, religious, cultural and social precepts – in accordance with National and International Ethical Guidelines and Standards.
For further questions and inquiries, you may contact the Patient Relations Office at locals 3034 and 3038.
Contact Us
Makati Medical Center
2 Amorsolo St. Legaspi Village
Makati City, Philippines 1229
MakatiMed OnCall 24/7: +632.8888.999
MakatiMed Emergency: +632.8888.910
URL: www.makatimed.net.ph
Admissions
Phone: +632.8888.999 locals 3000 and 3001
Location: Ground Floor Tower 1
Service Hours: Daily, 24 Hours
Sales Services
Phone: +632.8888.999 locals 3778 and 8708
Location: 6th Floor Tower 3
Email: [email protected]
Service Hours: 7:00 AM to 7:00 PM (Meetings strictly by appointment only)
MakatiMed respects a patient’s right to state and ensure his or her healthcare preferences ahead of time. You can make your decisions in advance, while you are healthy and composed. This helps your doctor(s) and loved ones carry out your medical preferences when you become unable to express or communicate them.
WHAT IS AN ADVANCE DIRECTIVE?
An Advance Directive is a patient’s instructions to his or her doctors and other healthcare workers, as well as his or her family and loved ones the type of care preferred should he or she become unable to make medical decisions.
WHAT IS A LIVING WILL?
A Living Will is a document that describes the type of medical treatment you want in certain situations. It comes into effect if you are terminally ill or permanently unconscious and is unable to express / communicate your medical wishes.
WHAT IS A DNR ORDER?
A Do Not Resuscitate (DNR) order is one type of advance directive. This allows you to decide NOT to undergo cardiopulmonary resuscitation (CPR) or other treatments which will try to revive you if your heart stops or if you stop breathing.
WHAT IS DECLARATION TO WITHDRAW OR WITHHOLD TREATMENT?
This is another form of Advance Directive by a patient, or relative of a patient, to withhold or withdraw life-sustaining procedures that will prolong the dying process. This declaration is made by a patient (or a relative of a patient) who is suffering from an incurable disease or injury or any other health circumstance where there is a high possibility that death will occur whether or not life-sustaining procedures are utilized, and where the application of such procedures will only serve to prolong the dying process.
WILL OTHER TREATMENTS BE DISCONTINUED WHEN A PERSON ISSUES A DNR ORDER?
A Do Not Resuscitate (DNR) order only means that cardiopulmonary resuscitation (CPR) will not be performed. It does NOT change the rest of the medical care plan. No other treatments will be discontinued unless the doctor and patient and / or family decide they want a treatment stopped (as in the case of declaration to withdraw or withhold treatment). Some treatments may also not be started if the patient, family, and physicians decide this ahead of time.
HOW DO I MAKE SUCH A DECISION?
Decisions such as these are difficult and you need to discuss these with your loved ones and caregivers, your doctor, and other members of the healthcare team. You may also want to talk with your clergy or religious leader, or any other trusted spiritual or emotional advisor.
REMEMBER THAT YOU CAN CHANGE YOUR DECISION AT ANY TIME BY TALKING TO YOUR DOCTOR.
If you decide that you do want a Do Not Resuscitate (DNR) order, you need to:
- Tell your doctor so he or she can write a DNR order in your medical record
- Consider whether you want to make the DNR order permanent. You can record this on paper, a wallet card or medical jewelry (bracelet or necklace) that you wear
WHAT IS A DURABLE POWER OF ATTORNEY FOR HEALTHCARE?
A Durable Power of Attorney is another type of Advance Directive. This document states who you choose to speak on your behalf about healthcare decisions if you cannot do so yourself.
SHOULD I BRING MY ADVANCE DIRECTIVE DOCUMENTS?
It is a good idea to have a copy of your Advance Directives with you for each hospital admission. Remember to tell your healthcare team and give a current copy to all involved, including your doctor.
WHO NEEDS AN ADVANCE DIRECTIVE?
Everyone is entitled to have an advance directive. It is important that your doctor and loved ones know about your healthcare wishes. The best time to put your wishes in writing is when you are in good health. These documents will help your doctor and family to know and honor your choices.
HOW CAN I MAKE OR CHANGE MY ADVANCE DIRECTIVE?
You can change or make a new Advance Directive at any time. Simply disregard the old one and create a new written advance directive. If you have questions or need help to put your choices in writing, you may contact Patient Relations Office at locals 3034 and 3038.
MakatiMed, in compliance with the Joint Commission International (JCI) standard for hospitals, values the highest quality of patient care and strives to provide a safe, effective and meaningful healthcare environment. We continuously provide competent and responsive healthcare services to achieve the highest level of satisfaction from our patients and visitors.
If you have concerns or complaints on patient care or safety, we encourage you to inform us. We would appreciate hearing from you.
Step 1: You may inform your nurse or doctor regarding your concern. They will do their best to address the situation.
Step 2: If the services provided by your nurse or doctor does not meet your expectations or address your needs, you may contact our Call Center (MakatiMed On-Call) through +632-88888-999. A Call Center Agent will immediately take note of your concern/complaint and refer the matter to our hospital administrator.
Step 3: If you feel that your concerns or complaints have not been addressed satisfactorily or sufficiently, you may choose to contact our Patient Relations Office at +632-88888-999 local 3034 or email [email protected]. A Patient Relations Officer will attend to your patient/visitor concern immediately.
Should you feel that your concerns have not been adequately addressed in spite of our best efforts, you have the option to express or communicate your complaints to the Quality and Safety Monitoring Department of the Joint Commission directly through +1-800-994-6610 or send in a feedback through [email protected]. You may find more details on sending feedback to JCI by visiting the link: http://www.jointcommissioninternational.org/contact-us/report-a-quality-and-safety-issue/.
The Patient Relations Office
Department Manager: Richelle B. Bumanglag, MD
Contact Us
Phone: +632.88888.999 local 3034
Email: [email protected]
Office Hours: 8:00AM – 12:00PM and 1:00PM – 5:00PM Mondays to Fridays (Except holidays)
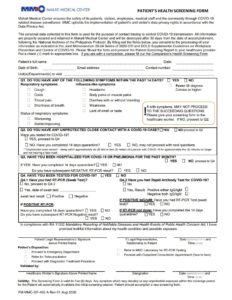
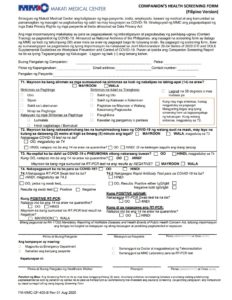
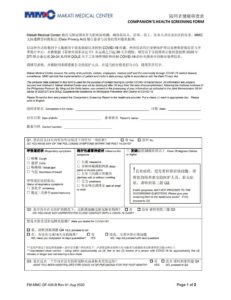
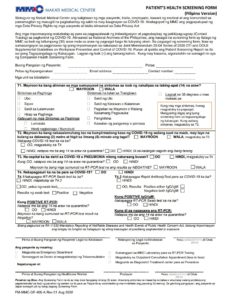
Click to download the forms
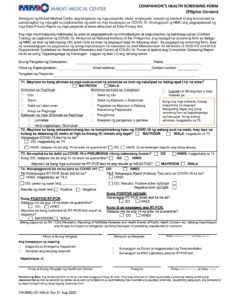
Patient’s Health Screening Form | Companion’s Health Screening Form |
Patient’s Health Screening Form | Companion’s Health Screening Form |
Patient’s Health Screening Form | Companion’s Health Screening Form |
Link to Online Screening Form
Online Screening Form | Online Screening Form |
Chinese Online Screening Form |