Psoriasis, though not life-threatening, can be life-altering. It can significantly disrupt daily life due to its physical symptoms and emotional impact. This chronic skin condition can affect people of any age or gender, and it occurs when the immune system triggers inflammation, causing new skin cells to form every five (5) to seven (7) days instead of the usual 28-day cycle.
Managing psoriasis is particularly challenging because flare-ups are unpredictable, and there is no cure. The condition presents as itchy, scaly patches of rash, commonly appearing on the knees, elbows, trunk, and scalp. In more severe cases, psoriasis can cause pain beneath the skin and lead to joint pain and swelling. Beyond the physical symptoms, the stigma surrounding psoriasis can take a toll on self-confidence and mental well-being, as the visible nature of the condition often leads to feelings of embarrassment or shame.
No two individuals experience psoriasis the same
Everyone’s experience with psoriasis can be distinct, shaped by their unique set of circumstances and risk factors. Angeli Eloise Torres-Paulino, MD, a board-certified Dermatology Specialist at Makati Medical Center (MakatiMed), assures patients that the range of treatment options is equally varied, allowing for personalized approaches tailored to meet each patient’s specific needs. “The reality is that although psoriasis is a condition that sticks around for life, treatments today are much better than they were even five (5) years ago,” the doctor reveals.
According to Dr. Torres-Paulino, examining what causes psoriasis in the first place is crucial to managing its symptoms. “Psoriasis can have a genetic predisposition, meaning if it runs in your family, you may have a higher chance of developing it. But some people get it without any family history, and the reverse
is also true,” the doctor explains. “Environmental triggers, such as stress, changes in weather, smoking, or infections, can also play a role. It all depends on how your immune system responds to these factors.”
Medical treatment options for psoriasis
For mild to moderate cases of psoriasis, doctors will typically prescribe topical treatments like creams and ointments. Over-the-counter moisturizers and emollients help control flare-ups by trapping moisture, while salicylic acid in lotions and shampoos removes scales and boosts the effectiveness of other treatments.
If the psoriasis is more severe or unresponsive to topical treatments, oral treatments suppress the immune system or slow down the rapid growth of skin cells. Additionally, injectable biologics have emerged as a powerful treatment option for moderate to severe psoriasis. These medications target specific parts of the immune system to reduce inflammation and can lead to significant improvements in symptoms. However, both oral and injectable treatments may have side effects, so regular monitoring by a healthcare professional is essential.
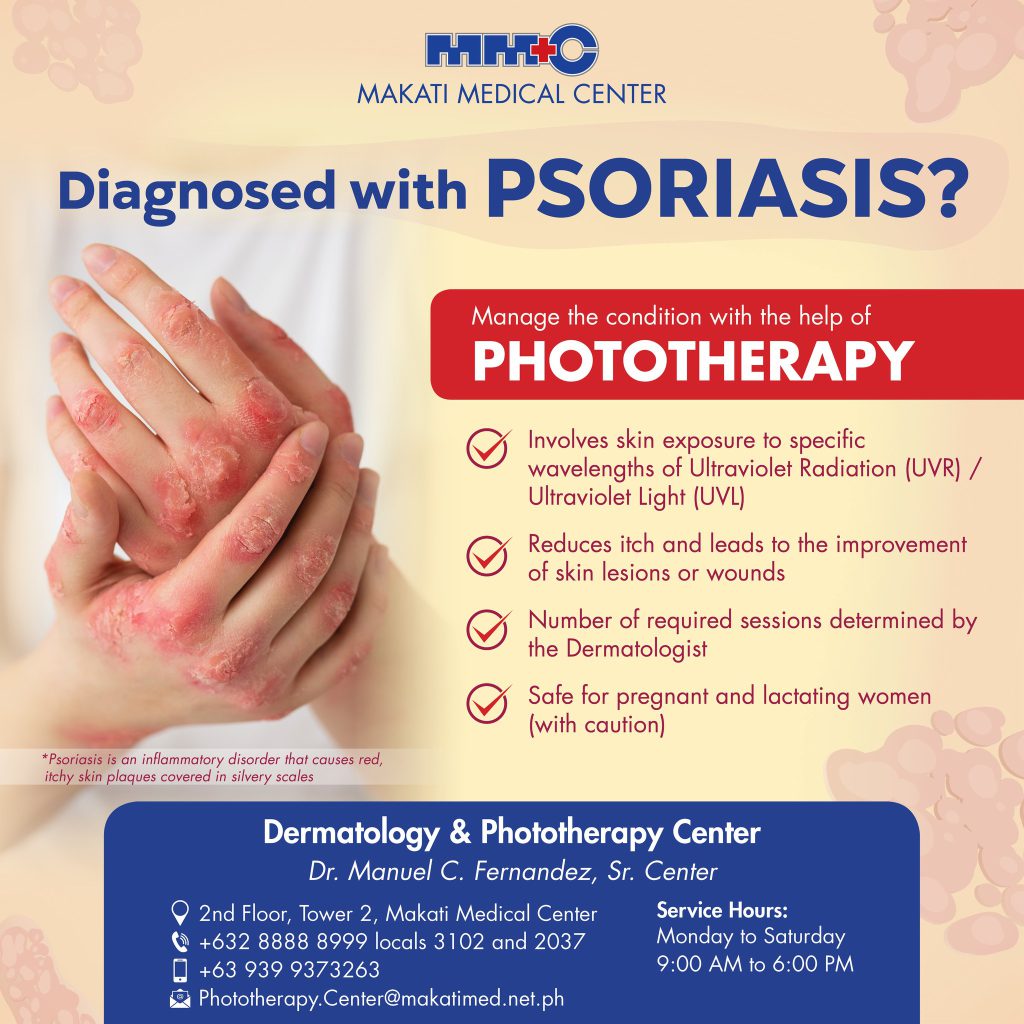
Phototherapy is another option that can be done under hospital supervision. This type of treatment is usually given to those with a weakened immune system or an ongoing infection, using UVB light or lasers to slow skin cell growth and ease symptoms.
Dr. Torres-Paulino emphasizes that combining more than one type of treatment may maximize effectiveness, especially because there is no one-size-fits-all solution when it comes to managing psoriasis. “For me, it’s important to treat the patient, not the diagnosis,” the expert shares. “It’s a matter
of finding the right treatment for you. If we find what works for you and keep your psoriasis in remission, you can potentially go through life as normal as possible.”
She also notes that once symptoms become under control, doctors will aim to gradually reduce the medication. The eventual goal is to maintain the condition with as little medication as possible.
Lifestyle changes to make for managing psoriasis
Alongside medical treatments, adopting a healthy lifestyle that involves avoiding smoking and alcohol and eating more vegetables and fruits plays a crucial role in managing psoriasis. This immune-mediated skin disorder is related to other conditions such as metabolic syndrome and cardiovascular diseases.
“There are findings that people who have metabolic syndrome or those who are obese and diabetic or have high cholesterol levels may develop psoriasis, especially if they have genetic predisposition,” Dr. Torres-Paulino says.
“If the person also has psoriasis, having diabetes, hypertension, or elevated cholesterol can also be a hindrance to controlling the condition. You will have better control of the skin disease when those factors are also controlled. Not only that, your risk of developing metabolic conditions like diabetes is also higher compared to the average individual. This is why people with psoriasis need to be more conscious about their general health.”
The Dermatology Specialist says that moderating the consumption of sweets and processed foods is advisable, as some studies suggest that an anti-inflammatory diet can be beneficial. It’s important to note that triggers can vary from person to person, so it’s helpful to keep track of any foods that may trigger flare-ups.
Dr. Torres-Paulino reminds patients that the best way to keep psoriasis flare-ups at bay is to continually work with a Dermatology Specialist. Regular check-ups allow for personalized treatment adjustments, ensuring that the approach remains effective as symptoms evolve and new triggers may emerge. This collaborative relationship can lead to more effective management of the condition, prevent complications, and help maintain overall health.
Clarifying facts about psoriasis is crucial for reducing the stigma and improving the quality of life for those affected. Dr. Torres-Paulino emphasizes that psoriasis is neither contagious nor the result of poor hygiene.
“Someone having psoriasis does not mean they’re dirty. In fact, they’re not even contagious at all—you can even hug people with psoriasis because you can’t get it by touching,” the doctor highlights. “Remember, psoriasis isn’t contagious, but awareness is.”
Article based on the MakatiMed Vodcast episode “Tackling Psoriasis” last September 28, 2022.
For the complete list of Makati Medical Center’s Dermatology Specialists click here. You may also reach us via MakatiMed On-Call at (+632) 8888 8999 or at [email protected].
Follow our social media pages for more health-related content and for the latest updates: https://www.makatimed.net.ph/social-media-pages