In 2013, Oscar-winning actress and filmmaker Angelina Jolie underwent a double mastectomy to reduce her chances of having Breast Cancer. Jolie explained in a New York Times opinion article that she chose to get the operation after discovering she carried a faulty BRCA1 gene that increased her risk of developing Breast and Ovarian Cancer. She notably has a family history of Breast Cancer, with her mother fighting the condition for a decade before passing away at 56.
For Makati Medical Center (MakatiMed)’s Frances Victoria F. Que, MD, who is the only Medical Oncology Specialist who practices cancer genetics and genomics in the Philippines, Jolie’s experience with finding cancer genes actually isn’t all that uncommon. Spotting the genes that are responsible for causing cancer is now easier thanks to genetic testing. This type of testing looks for inherited gene mutations that might put a person at a higher risk for hereditary cancers.
“We have about 30,000 genes in our body. Genes are made up of DNA and through testing, we look at the DNA sequences of cancer protection genes,” explains Dr. Que. “Most hereditary cancers are inherited through an autosomal dominant pattern. This means that if one parent carries a mutated gene associated with cancer, there is a 50% chance of passing it on to their child.”
With genetic testing services now also available at MakatiMed, you can preempt cancer similar to how the Tomb Raider star did. But how does it work exactly?
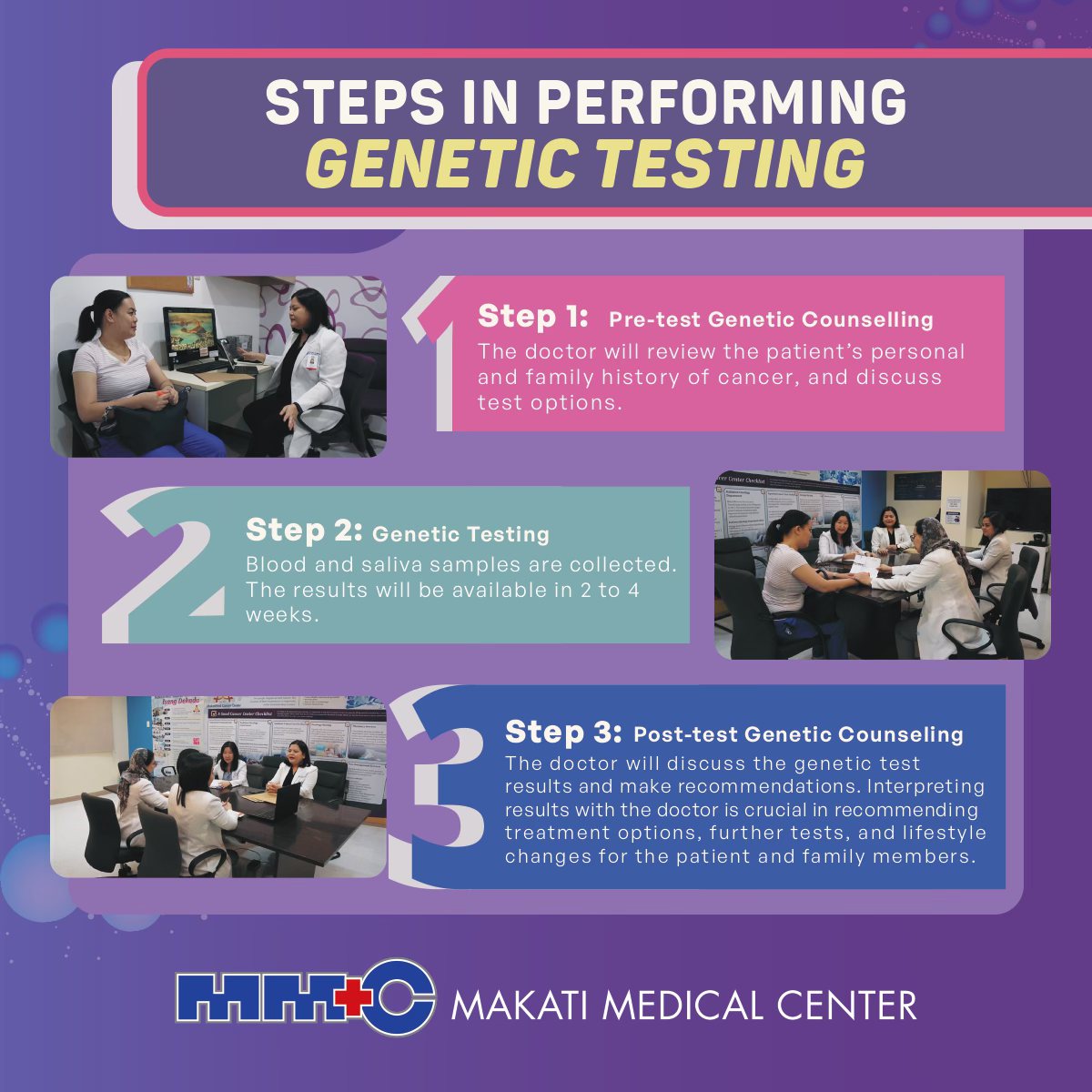
The testing process
The first step in genetic testing for cancer is figuring out who needs it in the first place. “Not all cancers are hereditary. Most cancers are what we call sporadic, meaning they happen by chance with risk factors that mainly include age, environment, and lifestyle,” the doctor says.
“Only 5-10% of cancers are hereditary. The most common that we usually encounter are affecting women. It’s typically caused by two cancer protection genes, BRCA1 and BRCA2, mostly associated with Breast and Ovarian Cancers as well as Prostate and Pancreatic Cancers. Other types of cancer that could be passed on are Colorectal and Endometrial Cancers.”
According to Dr. Que, genetic testing is recommended for adult patients who already have a cancer diagnosis or a strong family history of cancer. Once a need for genetic testing is firmly established, patients are directed to undergo genetic counseling. This is where counselors can discuss the specific tests that will be used, the potential risks and benefits of testing, expenses, and medical implications of test results.
The testing is usually done by getting a blood or saliva sample. These specimens will also be sent to labs abroad, where technicians will look for anomalies in the genes. The results will then be sent back to the healthcare provider for further analysis and discussion.
What happens after
Dr. Que says that genetic testing for those diagnosed with cancer can help inform them about the most effective treatment options for the patient. For example, young ovarian cancer patients who have BRCA1 are advised to have preventive removal of ovaries and fallopian tubes as early as 35 years old.
However, the expert is careful to emphasize that a positive result doesn’t mean you’ll automatically get cancer, especially if you got tested because of a family history of cancer. A positive result only shows increased risk, not certainty, and a genetic counselor can explain the results and suggest ways to lower your risk as well as your family’s.
Dr. Que adds that these counseling sessions can even become a family affair. “When we do testing for a patient, they need to understand that the benefits of the test will not just be for them as treatment or aiding in prognosis, surveillance, and monitoring. It also helps screen other family members who might be at risk.”
In certain cases, the doctor mentions that patients who do not have cancer but got positive test result may be advised to undergo risk-reducing surgical procedures and even chemoprevention tablets to decrease the risk of cancer.
“Genetic testing is meant to help people understand whether they need to undergo procedures like a prophylactic bilateral risk-reducing mastectomy or bilateral risk-reducing salpingo-oophorectomy, which reduces the risk of breast and ovarian cancer by about 90%,” she says, referring to Jolie’s procedure.
Dr. Que also recommends regular screenings. For instance, those who don’t have cancer but got the BRCA1 and BRCA2 are advised to have annual mammograms and breast MRIs as early as 25 years old to help detect tumors before they can be felt and before symptoms manifest—the stage where breast cancer is most treatable.
The expert also underlines managing cancer risk by adopting several lifestyle changes such as maintaining a healthy diet rich in fruits, vegetables, and whole grains, engaging in regular physical activity, avoiding tobacco products, and limiting alcohol consumption.
“One of the goals of genetic testing is to shift from reactive care—waiting for someone to get diagnosed with cancer and treat them—to proactive care where we’re able to preempt the disease molecularly by doing the tests, so we can take measures to decrease that cancer risk and even decrease the burden to our healthcare system, too” notes Dr. Que.
Article based on the MakatiMed Health Vodcast episode “Did I inherit cancer through my family? Find out through cancer genetics testing” last May 10, 2023.
To learn more about Genetic Counselling and Genetic Testing, visit MakatiMed Cancer Center at the 1st Floor Circular, Tower 1. You may also reach the Center at (+632) 8888 8999 local 7102 or 7122, or at [email protected].
Follow our social media pages for more health-related content and for the latest updates: https://www.makatimed.net.ph/social-media-pages/